Healing a Herniated Disc Naturally Involves Two Principles
- Limit movements and positions that exacerbate disc herniations
- Specific exercise that helps the disc heal and become stronger
Limiting or avoiding movements that aggravate disc herniations reduce inflammation, pain, and irritability.
This also allows the outer part of the disc to heal, where it’s herniated.
Proper exercise training improves the nutrition of the disc and strengthens the disc tissue, facilitating the natural healing process.
The discs between the vertebrae are avascular, they have minimal to no blood supply. In fact, the intervertebral disc is the largest avascular structure in the body. Consequently the discs obtain nutrients and get rid of waste by fluid diffusing through the endplates of the vertebral bodies.
Movement and exercise result in cyclic loading and unloading of the disc, promoting the diffusion of solutes through the vertebral endplates.
Exercise is essential for disc hydration, nutrition, and for maintaining the balance between water and proteoglycan content. The inside of the disc (nucleus pulposus) contains water and proteoglycans. Exercise maintains the balance between the two.
Research shows that exercise is required to maintain the health and function of lumbar discs.
This is a fact of healthy discs, that are not causing any pain.
If a disc is causing lower back pain, exercise is required to promote the healing process and to strengthen the disc so it can tolerate loading and activity.
Exercise improves disc hydration and proteoglycan content and increases disc height. Basically exercise improves disc health and strength. Just like exercise makes bones and muscles stronger, exercise makes lumbar discs stronger.
Exercises that help herniated discs heal naturally
- forward alternating lunge
- reverse alternating lunge
- bird dog
- fast walking with arm swing
- pull-up
- dead hang
- dip
- bridge
- prone press-up
This list is by no means exhaustive. It’s a great place to start. Each exercise loads the spine dynamically, maintains the lumbar spine in neutral, and engages the core.
The best types of exercise to heal a herniated disc naturally
The exercise should engage the muscles of the trunk and spine (core) with active movement.
So cyclic loading and unloading of the disc with movement is superior to loading the disc statically.
Fast walking or slow running have been shown to be beneficial for the disc. Both of these activities result in cyclic loading and unloading of the disc, with load sharing through the lumbar disc, joints, and muscles.
Fast walking and slow running increase the hydration and glycosaminoglycan content of the disc. The size of the disc is also increased with these activities.
Slow running or jogging will NOT be tolerated well with an acute disc injury. If you want to run, wait until pain has decreased by at least 80%. This may be 6-12 weeks after the onset of symptoms.
A larger, thicker disc with greater water and glycosaminoglycan content is a healthier, stronger disc.
Simply walking fast or running slow results in a stronger, more healthy disc.
A simple walking program will improve disc health. Walking promotes load sharing between the tissues of the lumbar spine, is the definition of dynamic loading, and decreases lower back pain.
Research shows that walking 90 minutes per week decreases the risk of developing lower back pain.
Walking, by itself, is preventative.
An entire rehabilitation program can be based on a walking program. A good goal is to build up to walking 90 minutes or more per week over the course of four to six weeks. Then maintain the walking program to reduce the likelihood of future lower back pain.
Walking and jogging are not the only types of exercise that improve disc health.
Any exercise that results in cyclic loading of the lumbar tissues, maintains the spine in a neutral position, and engages the core musculature is beneficial.
What exercises do I start with?
It’s best to start with the easier exercises first. Prone press-ups, bridges and bird dogs are three great exercises to start with.
How many sets and reps of each exercise should I do?
2-4 sets of 8-15 reps is a good range to work within.
How long should I do these exercises?
You should plan on doing these exercises for 6-12 weeks. Over the course of 6-12 weeks the exercises need to be progressed with additional volume.
You should also progress the exercises themselves. So 6 weeks from now you should be doing higher level exercises than the ones you started with.
You may be doing lunges and pull-ups opposed to bird dogs and bridges in 6 weeks.
Built for you programming to heal herniated discs
How do Herniated Discs Heal Naturally?
The process by which discs heal is called spontaneous regression
Basically the disc herniation decreases or completely goes away over a period of time. Herniated discs are more likely to undergo spontaneous regression when they’re more severe.
A disc that is completely extruded or sequestered has the best chance of spontaneous regression. This is good news. The worse the herniation is the greater likelihood your body will take care of it naturally.
When a disc herniates the inner part (the nucleus pulposus) pushes out through the annulus fibrosus (outer part of the disc). If the inside is pushed completely out ( disc extrusion) or pushed out and part breaks off (sequestered disc herniation) there is a good chance spontaneous regression will occur.
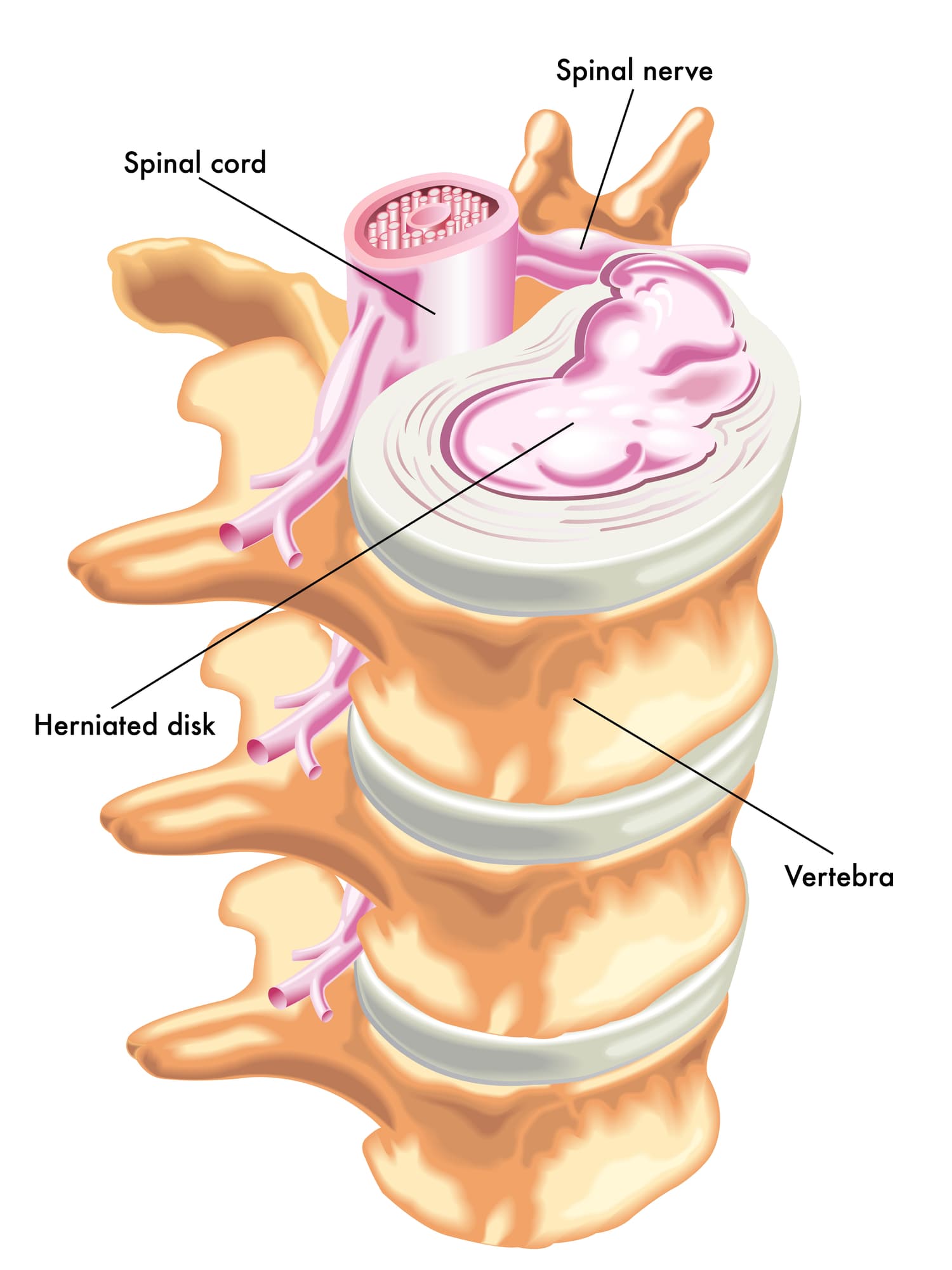
With smaller disc herniations spontaneous regression happens, just less frequently.
There are three theories that describe how spontaneous regression occurs.
- The herniated piece of nucleus pulposus dehydrates and shrinks.
- The posterior longitudinal ligament pushes the herniation back into the disc.
- There is an inflammatory and autoimmune response that basically cleans up the extruded nucleus pulposus.
It is likely that each of these proposed theories play a role in the healing of a herniated disc.
In some cases each method of spontaneous regression could play a role.
With the more severe disc herniations that result in sequestered disc material into the epidural space it’s likely that an inflammatory and autoimmune response is at work. It’s also likely that part of the disc material does dehydrate and shrink.
With a less severe disc herniation that does not result in sequestered nucleus pulposus, the posterior longitudinal ligament could push the herniation back in to a degree.
The take home message is; discs heal. The more severe the herniation the more likely spontaneous regression is.
Even if you have a disc herniation that doesn’t completely resolve on MRI you can be pain-free.
It’s likely your body does not completely heal small disc herniations because they are normal and not problematic.
Other considerations to heal a herniated disc naturally
Heat and Cold Therapy
- Cold Packs: Apply cold packs to reduce inflammation and numb acute pain.
- Heat Therapy: Use heat packs or warm baths to relax muscles and increase blood flow to the affected area.
Diet and Nutrition
- Anti-Inflammatory Diet: Incorporate foods rich in anti-inflammatory properties such as fruits, vegetables, whole grains, nuts, and fatty fish.
- Stay Hydrated: Drink plenty of water to maintain spinal disc health.
Supplements
- Omega-3 Fatty Acids: These can help reduce inflammation.
- Vitamins and Minerals: Ensure adequate intake of calcium, magnesium, vitamin D, and other nutrients that support bone and muscle health.
FAQ
How to heal a herniated disc naturally?
The best way to heal a herniated disc naturally involves two primary principles.
First, limiting movements and positions that exacerbate disc herniations. This generally involves limiting repetitive and end-range lumbar flexion.
Second, consistently completing exercise and movement work that facilitates healthy loading of the disc. This may involve lumbar stabilization training, simple walking programs, directional preference exercises, or a combination of all three.
How long does it take to heal a herniated disc naturally?
The medical literature shows that herniated disc pain usually lasts anywhere from 6 to 12 weeks. So a month and a half to three months.
There is a wide variance in healing time of lumbar discs. The medical literature states that herniated discs take anywhere from 5 to 22 months to heal. The average is 13 months, so right around 1 year.
Understand that healing in the medical literature is defined as an MRI showing no disc herniation where there had been a herniation. Many people heal without ever having a complete regression of a herniated disc.
And pain relief occurs LONG before a disc is considered healed based on an MRI showing a regression of a disc herniation. Pain decreases or goes away within 6-12 weeks while healing of the disc herniation takes on average 13 months.
Lots of people will still have herniated disc on MRI but will not have lower back pain or sciatica. This is important to understand.
How to naturally heal a herniated disc?
To naturally heal a herniated disc the disc herniation must not be loaded in a manner that exacerbates the disc.
Lumbar flexion and flexion combined with rotation increase compression and tensile loading through the posterior disc, where the disc herniates.
So flexion and combined flexion/rotation should be limited.
The disc does require loading via movement and exercise to heal though.
The key is loading the disc correctly. Exercises that involve cyclic loading of the lumbar tissues, maintains the lumbar spine in neutral, and engages the core are most beneficial.
If sciatica is present directional preference exercises will likely be beneficial to centralize leg pain.
Disc Healing and Exercise
- Discs heal through a process called spontaneous regression
- More severe herniations have a greater likelihood of regression
- Herniated discs can be pain-free even when they don't regress
- Discs require loading via exercise to heal and stay healthy
- Exercise facilitates the healing process
- Exercise increases disc loading tolerance and strength
References
Macki M, Hernandez-Hermann M, Bydon M, Gokaslan A, McGovern K, Bydon A. Spontaneous regression of sequestrated lumbar disc herniations: Literature review. Clin Neurol Neurosurg. 2014 May;120:136-41. doi: 10.1016/j.clineuro.2014.02.013. Epub 2014 Feb 25. PMID: 24630494.
Cunha C, Silva AJ, Pereira P, Vaz R, Gonçalves RM, Barbosa MA. The inflammatory response in the regression of lumbar disc herniation. Arthritis Res Ther. 2018;20(1):251. Published 2018 Nov 6. doi:10.1186/s13075-018-1743-4
Altun I, Yüksel KZ. Lumbar herniated disc: spontaneous regression. Korean J Pain. 2017;30(1):44-50. doi:10.3344/kjp.2017.30.1.44
Chiu CC, Chuang TY, Chang KH, Wu CH, Lin PW, Hsu WY. The probability of spontaneous regression of lumbar herniated disc: a systematic review. Clin Rehabil. 2015 Feb;29(2):184-95. doi: 10.1177/0269215514540919. Epub 2014 Jul 9. PMID: 25009200.